Interview with Paolo Decuzzi, coordinator of IIT’s ‘Nanotechnology for Precision Medicine’ Lab
The brain is a somewhat special organ, which not only contains the consciousness that makes us human and not only generates conditioned or unconditioned reflexes, but also has a controlling function over other vital organs. And it is precisely this extraordinariness that makes everything more complicated when we talk about therapies. Paolo Decuzzi – Director of the Laboratory of Nanotechnologies for Precision Medicine at the Italian Institute of Technology in Genoa – talks about his research into new methods of treating brain tumours, strokes and other diseases. A complex and fascinating tale, from which emerge the difficulties and paradoxes that the world of research, new materials and frontier medicine repeatedly encounter along the arduous road to progress.
Paolo Decuzzi is leading two ERC-funded projects whose topics are distinct from the point of view of biomedical applications. The ERC Consolidator ‘POTENT’, in the home stretch, aimed to develop nano- and micrometric devices to treat glioblastoma multiforme, one of the most aggressive brain tumours. The ERC Proof of Concept ‘Resolve’, on the other hand, aims to develop a technique for treating ischemic stroke.
What are the treatments for glioblastoma multiforme to date?
The peculiarity of brain tumours is that they are not on the list of the most frequent and widespread tumours, but are unfortunately extremely aggressive. There are no very effective treatments for these tumours and what is done today is to subject the patient to three successive steps of therapy. The first is surgical removal of the tumour mass, which has limitations because not only can the mass be difficult to reach, but it can also be diffuse and therefore not easily removed. Furthermore, one must take into account that the removal of brain tissue is not like that of other parts of the body, because the brain controls the other vital organs. Therefore, one of the problems that the neurosurgeon has to face is the safe removal of the maximum amount of tumour tissue, such that the brain capacity and quality of life of the patient is not damaged, but at the same time a rapid relapse is avoided. The second step is to subject the patient to cycles of radiotherapy, i.e. ‘illuminating’ the diseased tissue with radiation that damages the cancer cells. But this is never targeted, as the radiation inevitably also affects healthy cells or locally scleroticises the vascular system. The third therapeutic step consists in administering, sometimes even during radiotherapy, the drug temozolomide (TMZ), which is the only one approved for the treatment of these tumours, but has a very mild cytotoxic power. This three-step treatment protocol does, however, lead to a longer life expectancy of around 12 to 20 months, depending on the patient and the severity of the situation.
Here, new treatment methods were developed in the ERC’s ‘Potent’ project.
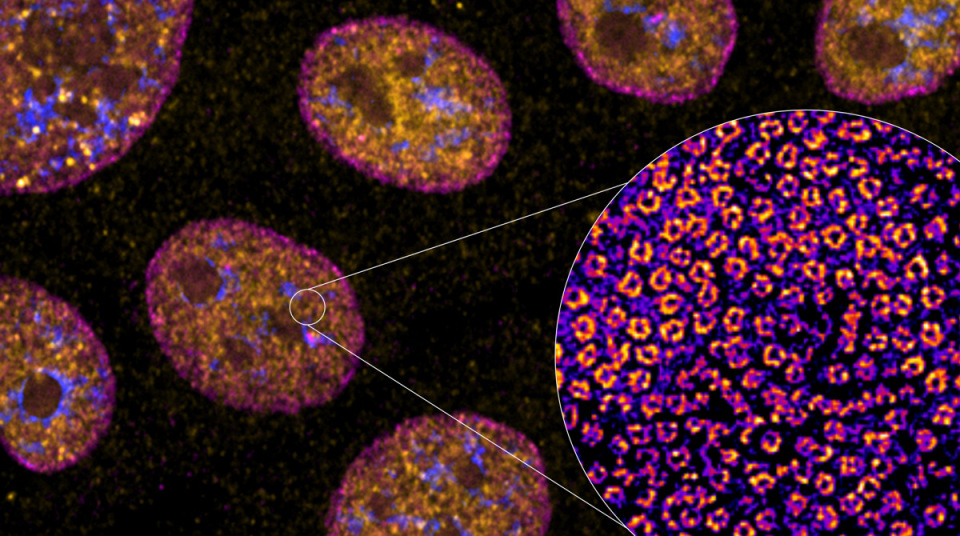
We followed two complementary paths in the project. The first involves the use of particles similar to our blood platelets in shape and size: they have a discoidal shape and their dimensions are of the order of a micron (one millionth of a metre). The particles developed are called Discoidal Polymeric Nanoconstructs. These particles are loaded with an extremely powerful drug, docetaxel (DTXL), and thus become the carriers of the drug.
What are these particles composed of?
They are made from two polymers (chains of molecules) identified by the acronyms PLGA and PEG. These polymers are well known to the world of scientific research and to the Regulatory Agencies for the approval of new drugs and biomedical devices (AIFA, EMA and FDA). The latter have the task of scrutinising the toxicity and efficacy of new therapies in order to authorise their marketing or not. The materials used are therefore conventional; what changes is the architecture, i.e. the way these materials have been ‘woven’ to make a one-micron disc-shaped particle. In other words, we have varied the physics, not the chemistry. This changes the results, but without having to follow a long series of steps to approve a new material and thus making the application accessible in less time. In any case, it is a few years from the end of the preclinical studies to the approval of the therapy.
Why precisely a disc-shaped particle the size of a micron?
In this project we have shown that this shape allows the particle to reach the diseased vessel more easily and with higher specificity: its geometric properties allow the particle not to deposit in healthy vessels, but to deposit more specifically in damaged ones. This allows us to significantly increase the amount of drug that can be deposited in the diseased tissue.
What is the second route followed during the project?
In parallel, we have developed another system, called micro-MESH, which is made from the exact same materials as the disc-shaped microparticles, but which follows a completely different approach. We no longer speak of a system that can be injected at the level of blood vessels, but one that can be applied to the surface of the diseased tissue, before or after removal of the tumour mass. As already mentioned, in the case of surgical removal, it is not possible to remove as much tissue as desired, as this would compromise the patient’s quality of life. This means that margins are always left, which can quickly develop and cause the tumour to recur. Therefore, this device was designed to be applied to the diseased surface. It is essentially an implant: in the same surgical operation in which the tumour is removed, this ìMESH is placed on the surface of the remaining diseased tissue.
How does this system work?
This device has been given the term ìMESH because it resembles a microscopic fisherman’s net. In fact, it is as if a fisherman’s net were to be deposited on the tumour, the aim of which is to fish out the diseased cells. In the threads of this net, either the drug or nanoparticles loaded with the drug, or even both, are deposited: the use of nanoparticles allows for a more targeted administration of the drug, and they are especially necessary when the drug being used is unable to reach the inside of the diseased cell on its own, as it degrades rapidly; in this case, the nanoparticles are able to transport it directly into the cell. Therefore, by depositing both the free drug and the nanoparticles loaded with a different drug on the meshwork, we are able to carry out a combination therapy, so as to attack the neoplasm from several fronts. The characteristic feature of ìMESH is, like the fisherman’s net, the ability to easily change its shape, resulting in a very flexible system that can conform to the surface on which it is deposited. Precisely because of these characteristics, it is able to release the drug from the surface to the inside of the diseased tissue.
What stage has been reached in the trials?
Trials of the platelet-shaped nanoparticles are continuing, and we are currently conducting preclinical experiments to confirm their efficacy. On other tumour types, we have already observed the incisiveness of this application, for instance on breast cancer. With regard to the mesh device, on the other hand, we have a patent and the first scientific work under review. In the case of ìMESH, we have completed the pre-clinical trials. In particular, we have carried out two types of experiments, using not only what are called conventional cell lines (laboratory cell samples), but also on authentic cells taken from patients and provided to us by our collaborators at San Raffaele in Milan. These cells allow us to have more accurate data regarding the biochemical and biophysical properties of the disease.
What has been observed from the pre-clinical trials?
In cases where we did not remove the tumour mass and applied ìMESH to the surface of the tumour, life expectancy in preclinical experiments was three times that of conventional treatment with TMZ. In cases where the tumour mass was removed, up to 250 days after the experiment, survival was 100%. In humans, this would suggest total remission of the disease for many years. For ìMESH treatment, DTXL was used in combination with a conventional anti-inflammatory drug.
How to achieve clinical application?
In this project, although not included in the ERC, a group of molecular biologists specialising in brain tumours from San Raffaele in Milan and a group of paediatric neurosurgeons from Lucile Packard Children’s Hospital at Stanford University are collaborating with us. Developing these activities in collaboration with biologists and ‘clinical scientists’ is crucial, to accelerate the migration of new technologies to the clinic. This helps turn beautiful scientific work into a technological object that can be effectively used to improve the quality of life, or even save the lives, of hundreds of thousands of people.
Would these potential new therapies also work on other types of cancer?
The studies we do are applied to brain tumours, because the European project we won was specifically about ‘Brain Tumor’. However, the approach can be applied to other neoplasms, such as colorectal cancer. In order to make the application more flexible, we are trying to modulate the ìMESH to provide different functionalities and make it applicable in different areas. We are looking at different applications not only for scientific interest, but also because a versatile device would be of more interest to pharmaceutical companies, as the pool of potential customers would increase significantly. In general, brain tumours, while not rare diseases, are much less common than other neoplasms. And unfortunately, when it comes to a small number of patients, the economic return is minimal for pharmaceutical companies and sometimes the investment is not very worthwhile.
PLGA and PEG are the two polymers of which both the disc particles and the ìMesh are made. Why was it decided to work on the architecture of these already known polymers and not on the use of other new polymers?
PLGA has been used in biomedical applications for over 20 years, during which time many other polymers have been developed, sometimes even better than PLGA at a preclinical level. For example, PCL has the characteristic of degrading much more slowly and would therefore guarantee a much longer drug release. However, no one is bothering to do in vivo studies on humans with new polymers, because the Regulatory Authority would rightly first ask to demonstrate what happens in terms of the degradation process and the products of the process itself. Having demonstrated that the polymer per se is safe, only then could we start with the clinical trial of the ‘polymer plus drug’ complex. This alone would therefore be a very expensive clinical trial, which could only be justified if the new material were orders of magnitude (10 – 100 times) superior to PLGA.
A few words about the ongoing Proof of Concept project.
As for the ongoing Proof of Concept, the application still involves the brain, but in this case it concerns the treatment of ischemic stroke. The platelet-shaped discoidal particles we have been talking about, having the ability to circulate for a long time propelled by the blood, have been proposed as ‘blood vessel scavengers’: when there is a blockage in the vessel, they dissolve the ‘plug’, allowing rapid recanalisation and new blood circulation, which prevents the death of neurons and the resulting permanent damage. The problem with stroke or embolism in general is determined by the time one has to intervene. The health worker who picks up the patient from home and transports him to hospital has the ability to understand whether it is actually a trivial migraine or a stroke in progress, but has no means of diagnosing it accurately: the patient has to be taken to hospital and undergo a CT scan, but this can take up to a few hours and in the meantime the clot can grow and cause permanent brain damage. The idea is therefore to make the application of the discoid particles so simple and without side effects that the healthcare provider can immediately inject the solution before the patient even arrives at the hospital. This has already been demonstrated in vitro using donor blood. The Proof of Concept underway aims to demonstrate this on a preclinical level as well. To do this, we have connected with one of the best known groups in this field in Europe, which is located in France at the University of Cain, and we are collaborating with the Galliera Hospital in Genoa. Due to the Covid-19 pandemic, activities came to a halt between March and July, but we have now restarted and are moving forward. We expect to finish this activity by the autumn of 2021.