By Velia Siciliano, PI of Synthetic and Systems Biology for Biomedicine Lab, IIT
How does the body know what is safe, when to defend? How does it know when to stop once the attack has mounted? In a healthy immune system, balance is everything.
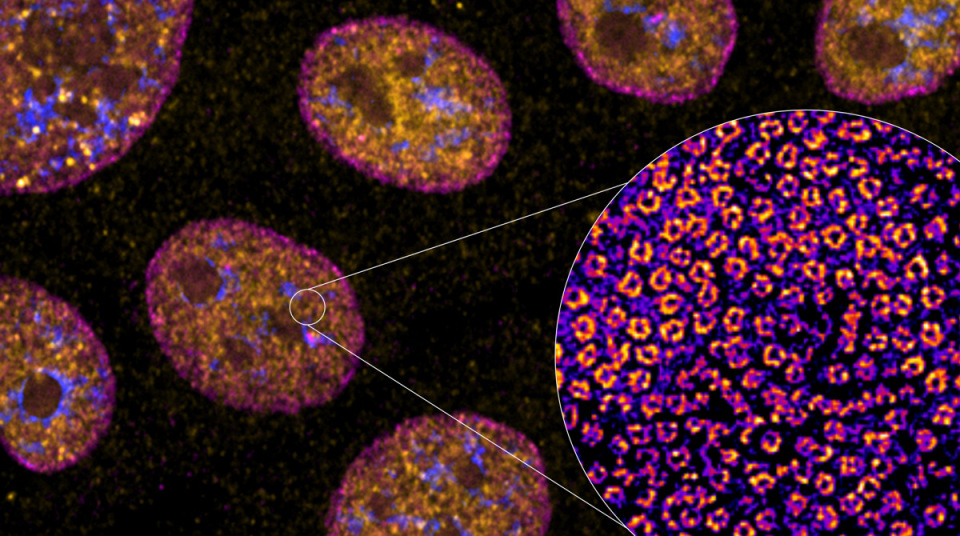
The body must attack pathogens yet avoid turning its weapons against itself. This delicate equilibrium depends on regulatory T cells (Tregs), a specialized subset of T immune cells that suppress excessive or misdirected immune responses. T cells are named with a T, because they mature in the thymus gland. Without them, the immune system’s brakes fail, leading to autoimmune diseases such as type 1 diabetes, multiple sclerosis, and IPEX syndrome (a genetic condition where the immune system attacks its own body organs).
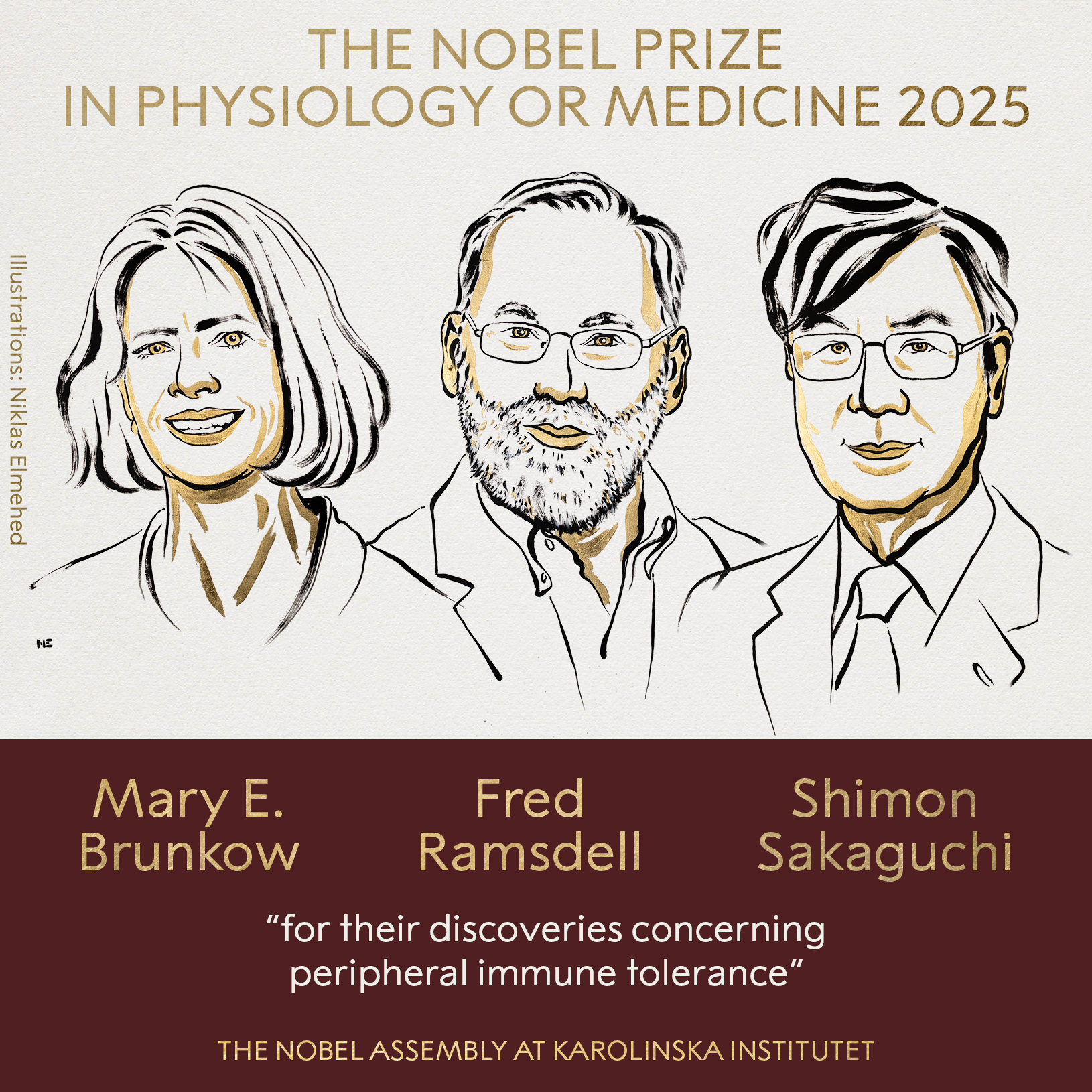
The existence of these “peacekeeping” cells was first uncovered by Shimon Sakaguchi, who showed that removing a small subset of T cells caused catastrophic autoimmunity in mice.
His work showed that the immune system has active self-regulation mechanisms even outside the thymus, preventing immune cells from attacking the body’s own tissues. This discovery revolutionized the understanding of immune tolerance and, as a result, reshaped the entire field of immunology.
Years later, Mary E. Brunkow and Fred Ramsdell identified the missing genetic piece: FOXP3, a transcription factor whose mutation caused the fatal IPEX syndrome. Their discoveries demonstrated that FOXP3 is the master regulator of Treg development and function, the molecular signature of the immune system’s restraining arm.
Together, Sakaguchi’s identification of Tregs and Brunkow and Ramsdell’s elucidation of FOXP3 formed the foundation of modern immune tolerance research, the branch that studies the ability of the immune system to recognize the body’s own cells and tissues as “self” and therefore not attack them. Their collective work not only explained why autoimmunity occurs when regulation fails, but also opened new therapeutic frontiers, from restoring tolerance in autoimmune disorders and transplants to modulating it in cancer immunotherapy.
Today, that insight underpins a new generation of cell therapies. By isolating and expanding a patient’s own Tregs, or even engineering them with specific antigen receptors, scientists can selectively turn down harmful immune responses, offering hope for autoimmune diseases, organ transplants, and inflammatory disorders. Conversely, in cancer or chronic infection, where the immune system becomes overly restrained, the same pathways explain T-cell exhaustion, a state of dysfunction driven by persistent suppression.
Thus, the molecular logic uncovered by these three laureates bridges basic immunology and modern medicine: understanding how to apply the immune system’s brakes or release them now defines some of the most promising frontiers in therapy.